Florida stroke assessment
The Florida stroke assessment helps you quickly identify a patient experiencing a stroke, as there is no time to waste in getting help for a stroke victim. A stroke is marked by the sudden onset of a droopy face on one side, weakness of the arm or leg on one side of the body, and the inability to speak.
-
 (If you have not done so already) Access the EHR module in the ESO Suite.
(If you have not done so already) Access the EHR module in the ESO Suite.
-
Do one of the following.
-
(If you are already working in the ESO Suite) Click the Home icon in the upper left corner of the screen.
-
 (If you have not yet logged in) Log in to the ESO Suite.
(If you have not yet logged in) Log in to the ESO Suite.
-
In a web browser, go to https://www.esosuite.net/EsoSuite.
The ESO Suite login screen appears.
-
Enter your user name, password, and agency name, then click Let's Go.
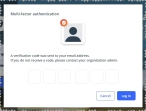
If MFA is enabled, the Multi-factor authentication dialog box appears, displaying one or more methods you can use to verify your login credentials. The number of methods that appear in the dialog box depends on what MFA methods your ESO Suite administrators enabled in the Admin module.

Click graphics
to open them.Information on enabling MFA and specific MFA methods is available in the Admin module online help, in Configure multiple-factor authentication.
Note: If your ESO Suite administrators have disabled MFA ("opted-out"), this dialog does not appear.
-
(If the Multi-factor authentication dialog box appears) Depending on which buttons appear in the dialog box, verify your login in one of the following ways.
 With an authenticator application.
With an authenticator application.
-
Click MFA verification via authenticator app.
The dialog box updates with boxes for entering the numbers of the authentication code, and the ESO Suite sends an authentication code to the authenticator application installed on your device.
-
Open your authenticator application and note the authentication code currently displayed.
-
Enter the authentication code displayed in the authenticator application.
-
Click Log In.
 With a text message (SMS).
With a text message (SMS).
-
Click MFA verification via SMS.
The dialog box updates with boxes for entering the numbers of the authentication code, and the ESO Suite sends an authentication code to the phone number recorded in your PM records and identified with MFA codes.
-
Enter the authentication code sent to your MFA-registered phone number.
-
Click Log In.
 With an email message.
With an email message.
-
Click MFA verification via email.
The dialog box updates with boxes for entering the numbers of the authentication code, and the ESO Suite sends an authentication code to your agency or department email address, recorded in your PM records.
-
Enter the authentication code sent to your agency or department email address.
-
Click Log In.
-
-
The ESO Suite landing screen appears.

Click graphics
to open them.Note: If MFA is enabled, you can access and manage your MFA options through the PM module, on the Settings > Account page, as described in Manage a user account. If your agency or department has enabled MFA but has not purchased the full-featured version of the PM module, you can access your own MFA settings by clicking Change my Multi-Factor Authentication settings on the landing screen, then using the Settings > Account page that appears. If your agency has not enabled MFA, the Change my Multi-Factor Authentication settings link does not appear on the landing screen.
-
-
On the top side of the home screen, click EHR.
Tip: If your screen or browser window is too narrow to display all your agency's ESO Suite module icons, an options icon appears on the right side of the icon bar. If you click the options icon, a menu appears containing additional module icons.
The EHR screen appears, displaying a list of patient records in the EHR module. The most-recent records appear at the top of the list.
Different record status icons can appear in the list.
Icon Status Unlocked/DraftThe patient record exists in the ESO Suite database, and all crew members listed in the patient record may edit all fields in the record. ESO Suite administrators and personnel with security roles of either
EHR SupervisororEHR Managercan edit non-clinical fields.MobileThe patient record exists on the mobile device, and has not been synchronized with the ESO Suite database. ESO Suite administrators, personnel with security roles of either
EHR SupervisororEHR Manager, and all crew members listed in the patient record can only access a print view of the record.Once the Mobile record synchronizes with the ESO Suite database. the record reflects its current status.
LockedThe patient record exists in the ESO Suite database, and is locked. Only non-clinical fields can be edited by crew members listed in the patient record, ESO Suite administrators and personnel with security roles of either
EHR SupervisororEHR Manager.
-
-
 (If you have not done so already) Add a new patient record, or search for the existing patient record you want to work with.
(If you have not done so already) Add a new patient record, or search for the existing patient record you want to work with.
Information on adding or opening a patient record is available in Add a patient record and Search for a patient record.
The patient record opens and displays the Incident tab, with the Response bookmark selected in the left pane. Fields appear in the right pane for specifying basic information about the incident
If you manually created a new patient record, the Incident Number and State Tracking Number fields populate automatically with ESO Suite-assigned values. You must enter data in all other required fields.
If you imported data from a CAD system, the Incident Number field populates with the data from that source. Other fields in the EHR module may also populate from these sources, depending on what data was recorded in them before the data was imported into the EHR module.
-
At the top of the page, click the Forms tab.
The contents of the Forms tab appear, listing all the forms your ESO Suite administrator has enabled in the Admin module.
-
Click Florida Stoke Assessment.
The Florida Stroke Assessment dialog box appears, with the Times bookmark selected in the left pane.
-
 Record the assessment times.
Record the assessment times.
-
For Time Performed, click the number pad icon to the right of the field, then enter the appropriate numerical values from the number pad dialog box that appears for the time you evaluated the patient using the Florida stroke assessment.
The unlabeled green time field at the top the dialog box updates to reflect the time you performed this assessment.
-
For Date, click the calendar icon on the right end of the field and select the appropriate date from the calendar that appears for the date you evaluated the patient using the Florida stroke assessment.
-
For Onset Time, click the number pad icon to the right of the field, then enter the appropriate numerical values from the number pad dialog box that appears for the time someone noticed the patient experiencing stroke symptoms.
-
For Date, click the calendar icon on the right end of the field and select the appropriate date from the calendar that appears for the date someone noticed the patient experiencing stroke symptoms.
-
For Last Known Well, click the number pad icon to the right of the field, then enter the appropriate numerical values from the number pad dialog box that appears for the time someone last knew the patient was well, before the stroke occurred.
-
For Date, click the calendar icon on the right end of the field and select the appropriate date from the calendar that appears for the date someone last knew the patient was well, before the stroke occurred.
-
-
 Note the results of the assessment.
Note the results of the assessment.
-
In the left pane, click the Assessment bookmark.
The right pane scrolls down to the top of the Assessment section of the page.
-
Record the Florida stroke assessment findings in one of these ways.
 Record the first set of assessments.
Record the first set of assessments.
-
For Level of Consciousness / Speech / Orientation, click the field or the list icon to the right of the field, then select the appropriate single option from the menu that appears to indicate the patient's condition in these areas.
-
For the following fields, click Left, Right, Bilateral, or Normal, depending on whether the patient meets the criteria below for normal function.
Field Criteria for Normal Facial Droop
The patient's face moves symmetrically on both sides when they smile.
Visual Fields Decrease
The patient has not lost an area of vision in their visual field. Vision field loss usually occurs on the same side as any weakness in the face, arms or legs.
Horizontal Gaze
The patient's eyes can follow an object from side to side, equally well in both directions, without turning their head.
(Open Eyes) Arm Drift and (Closed Eyes) Arm Drift
The patient can close their eyes and hold both arms out with palms up for 10 seconds, or whether one arm drifts down compared to the other arm.
(Open Eyes) Leg Drift and (Closed Eyes) Leg Drift
The patient can stand on one leg, then the other, for five seconds, without the raised leg drifting downwards.
(Open Eyes) Arm Sensory Decrease and (Closed Eyes) Arm Sensory Decrease
The patient has full arm tactile sensation (touch) or proprioception (awareness of body position). Sensory deficits can include the reduced ability to feel touch, pain, temperature, position, or the ability to recognize objects you are holding. It can also reduce
the ability to discriminate textures, weights, shapes, and sizes, to grasp and manipulate objects without vision.
(Open Eyes) Leg Sensory Decrease and (Closed Eyes) Leg Sensory Decrease
The patient has full leg tactile sensation (touch) or proprioception (awareness of body position). Sensory deficits can include the reduced ability to feel touch, pain, temperature, position, balance, weight bearing and load detection. This in turns affects load detection and gait symmetry, particularly in the push-off phase, which influences variance in stride length, gait speed, and walking endurance.
(Open Eyes) Arm Coordination Decrease, and (Closed Eyes) Arm Coordination Decrease
The patient has full bi-manual grip forces, can hold objects with both hands, and can exchange an object between the hands without the object falling or slipping from the hands.
(Open Eyes) Leg Coordination Decrease and (Closed Eyes) Leg Coordination Decrease
The patient has full bi-manual weight support, stride length, gait speed, and symmetrical gait pattern and cadence.
-
-
-
 (Optional) Add another set of assessments.
(Optional) Add another set of assessments.
-
At the top dialog box, click the Add button.
A new green time button appears between the left of the Add button, and a set of new, blank fields appears in the right pane of the dialog box for recording another set of assessments.
-
Repeat steps 5 and 6 to capture the data for the new assessment.
-
Repeat steps a and b above to continue adding more assessments as needed.
Corresponding green time buttons appear to the left of the Add button for each new assessment.
-
(Optional) At the top of the dialog box, click any time-performed button corresponding to the set of assessments you want to view.
The fields in the dialog box populate with the data specific to that assessment.
-
-
 (If necessary) Delete a set of assessments.
(If necessary) Delete a set of assessments.
-
At the top of the dialog box, click the time-performed button corresponding to the set of assessments you want to delete.
The fields in the dialog box populate with the data specific to that assessment.
-
Scroll to the bottom of the dialog box and click Delete Form.
A confirmation dialog box appears.
-
Click Delete.
The EHR module deleted all the data recorded for the specific assessment time, and the time-performed button disappears from the top of the dialog box.
-
-
Click OK.
The dialog box closes, and a green triangle appears in the upper right corner of the form button, to indicate that data exists in this form.